
Author: David J. LeClercq, President & CEO
Happy Quitters Day!
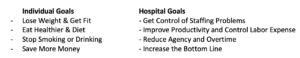
Research and polling indicate New Year’s Resolutions typically end the week between January 25th and February 1st, and many well before. Like ourselves, hospitals often have the same goals to improve from the previous year. Oftentimes, January 1st marks the beginning of either the Budget Process or the beginning of the “This is the Year”! With that come institutional goals similar to our own personal ones…
The question begs, why do we always have to go through this? The abrupt answer is “because what we are doing is not working.” Fitness coaches will preach the key to success is to turn these resolutions into a new lifestyle, like hygiene. You follow the daily plan, monitor progress, and solidify from a new activity to a normal daily occurrence. The difference with healthcare is we don’t really know the “drill” because each year we have to vow to do better…which means it isn’t working. Imagine if your trainer gave you a plan, you followed it, and every January 1st you set goals that were similar to last year’s. If that were the case, you would probably get a new trainer. C2 HEALTHCARE will set you on a course so that you don’t make “resolutions” every new year.
The approach of C2 HEALTHCARE is very straightforward. Instead of submitting written recommendations to leadership and projecting improvement opportunities, we create an environment of fiscal accountability and continuous improvement by implementing the OPTIX Reporting System, a cost-based planning and labor analytics system. Combining our planning and daily management analytics, we work closely with front-line managers to create standards and help them to maintain and improve on these standards throughout the fiscal year. From our Boot Camp for Managers to our ongoing one-on-one and group coaching sessions, managers are given department specific management techniques they can immediately apply to their operations with confidence. Quite simply, we train your managers to become “small business owners” keeping one eye fixed on quality and the other eye on cost.
In terms of financial results, labor expense reductions range from 7% to 15% without the use of layoffs. Every organization has varying degrees of opportunity; however, we have found our approach, even in different healthcare markets, consistently exceeds expectations as managers learn to manage effectively.
In terms of management results, the outcome is a fine-tuned management team constantly working together towards the goals of the institution. At the individual level, managers become empowered: they are well informed, financially savvy, and possess the ability to make staffing and program changes based on daily reporting.
Hospitals Need to Reach “Peak Performance” Now More Than Ever
C2 HEALTHCARE can help. We have an unrivaled history of relationships and best practices for every hospital and practical management approaches to help your front-line leadership turn your “resolution” into lasting results!
For more information, please go to www.C2Healthcare.com or call us at 877-294-3500 to schedule a complimentary opportunity analysis.

Author: Betsie Sassen, R.N., M.S.N.
The Extent of the Problem
It is a perfect storm. The COVID-19 pandemic struck and eroded an already frail and thin nursing workforce. Nurses left hospitals in droves for many reasons, including fear of contracting COVID-19, challenges with children learning remotely at home, opting for early retirement, alternate employment options (including agency nursing), and burnout. Hospitals had nowhere to turn to staff their beds, so they turned to travelers, overtime, retention bonuses, sign-on bonuses, crisis pay, incentive pay, etc. Out of those options, a popular decision for many nurses was to leave the hospital for agency or travel nursing. Currently, a critical care agency nurse can be billed at $200/hour, which is over $416,000 a year for an $80k position! Before COVID-19, a typical agency contract was two times the average hourly rate of a nurse. Now the agency rates are three to even four times the average hourly rate.
While the third surge of COVID-19 is starting to subside, in most regions of the country, one would think the reliance on agency and the potpourri of premium pay should start to go down as well. But, to add insult to injury, the vaccine mandate that is beginning to be imposed is driving out thousands of nurses and other healthcare workers, and this will continue to fuel the need for agency and premium pay to keep beds open and services intact.
The nursing shortage is likely here to stay, and it was exacerbated by COVID-19 and the vaccine mandates that followed. The question becomes where do we go from here? Agency and exorbitant premium pay are not long-term solutions. Here is what C2 Healthcare is hearing from some of our clients and how we can help.
New Models of Care: Hospitals realize they may never return to “business as usual,” and old and new nursing models are being revisited and explored.
The Team Nursing model is re-emerging. This can include one Registered Nurse, one Licensed Practical Nurse, and one Certified Nursing Assistant to care for a group of 9-12 patients with everyone having specific duties within their scope.
Another model that is emerging is the Virtual Nurse. This model relies on videoconferencing technology. The virtual nurses monitor the unit from a remote center with dedicated devices in each room. The Virtual Nurse is responsible for 18 patients and participates in daily rounds and then is responsible for all communication such as obtaining lab results, reviewing charts, patient discharges, pharmacy, dietary, care management, and anything else that the bedside nurses request. This model currently exists at MercyOne in Des Moines and appears promising and something to keep an eye on.
Stop Gaps
Many challenges such as staffing shortages and the sheer cost of staffing have caused hospitals to close beds, which is never the desired strategy. Several hospitals have resorted to pulling nursing staff from their Clinics and Surgical Areas to work the inpatient nursing units. Not only does this fill a critical need, but it fills it at less cost. Hospitals are also pulling nurses with active licenses from Case Management, Education, and other areas to help with patient care. Sign-on bonuses, crisis pay, and retention bonuses have also been popular to attract and retain staff.
Additionally, hospitals are creating their own In-House Contracts where staff are obligated to work 8-10 shifts per pay period and receive an attractive incentive in addition to their base rate. That incentive amount increases for the night shift and weekends. While these In House Contracts are very expensive, it has helped some hospitals keep Agency nurses out, which is far more costly.
Hospitals Need to Reach “Peak Performance” Now More Than Ever
Whether it is a new Model of Care or creative Stop Gaps, hospitals need to become increasingly agile with the ability to adapt to long-term challenges. To emerge out of this crisis, hospitals will have to operate at high efficiency (“top of the license”), pay overly competitive rates, and provide high octane Quality and Service. The solution we are implementing is Peak Performance!
C2 Healthcare can help. We have an unrivaled history of relationships and best practices for every hospital and practical management training and tools to help your front-line staff manage at their Peak!

To our hospitals, friends, and colleagues in Louisiana, Mississippi, and Florida – you are foremost in our thoughts and prayers. We are standing by to help in any way.

Author: Chris Falls, C2 Healthcare
Nurses account for 30% of hospital staff, the largest group. Naturally, and rightfully so, the predominant media focus has been on these front line workers responsible for direct patient care.
However, this is not the only critical group impacted by a year-long epidemic. While perhaps not literally front-line, the ripple-effect stress on Radiology Technicians, Food Service Workers, Environmental Service Workers, and technical and support staff has had significant impact as well. Add to this a higher employment vulnerability to declining patient populations and we have an employee experience with compounded safety and financial stress. Perhaps appropriate recognition for this group is overdue.
While nothing can replace the direct expression of gratitude on a personal level, one effective indirect method we are seeing hospital managers use to combat burnout successfully is to solicit participation on a broader problem-solving committee. By placing confidence in these staff members to identify and resolve an operational constraint in the department or hospital, managers not only demonstrate trust and appreciation for what these individuals have to offer, but also build a sense of ownership and self-worth around an ability to initiate a positive outcome on their environment. The idea isn’t to form a committee just to form a committee. It’s to appreciate and re-engage these unsung heroes in a way that sustains their leadership by allowing them to internalize the benefit of a tangible positive outcome they created.
While nursing deserves our heartfelt appreciation, we wanted to extend an idea for supplemental support for staff that may be overlooked. They need and deserve recognition as well, for the benefit of everyone.

Author: Maggie Mahowald, Management Consultant C2 Healthcare
With more than 3.8 million registered nurses nationwide, nurses comprise one of the largest segments of the U.S. workforce. The backbone of many hospitals. not only do nurses serve at the bedside; they also represent about 25% of leadership roles in most organizations.
While the Covid-19 pandemic certainly had a global impact, one of the most affected groups is healthcare workers. They have had no choice but to show up, day in and day out, putting the calling of their profession above their own safety. Over the past year, nurses have picked up extra shifts to support their peers and provide quality patient care. However, all of this comes with a cost, both financial and personal.
This past year has put even more strain on a group that has historically struggled with burnout and turnover. Additionally, the allure of high-dollar travel assignments has tempted some nurses to exit their home organizations, leaving hospitals scrambling to backfill positions and compete financially.
As of October 2020, the national average for nurse turnover rates was 8.8 % to 37.0%, depending on geographic location and nursing specialty. Bringing Agency Nurses into an organization can cause added stress as core nurses are aware that their counterparts are being paid a premium to do the same job.
C2 Healthcare believes in hiring the right complement of staff that will allow your organization to expand and retract to match the fluctuating volumes experienced throughout the year. We take a close look at the use of Premium Dollars such as Overtime, Agency, and Extra Shift Incentive to aid in hiring decisions that get your staffing where it needs to be.
We have had the privilege of hearing the inspiring stories of our hospitals coming together throughout this pandemic. Nurse leaders have juggled the increased strains on their staff both in and out of the workplace. This year, the American Nurses Association has extended National Nurses Week and named May – Nurses Month. The World Health Organization has declared 2021 Year of the Nurse. C2 Healthcare is honored to take this opportunity to celebrate all of the nurses we have the opportunity to work with.

Author: Betsie Sassen, R.N., M.S.N.
During the peak of COVID-19, Med Surg floors were being staffed as Progressive Care floors, Emergency Rooms were staffed like Intensive Care Units, Progressive Care floors were staffed as Intensive Care Units, and Intensive Care Units were almost staffed at 1:1 RN to patient ratios. Essentially all units were staffed up by an additional nurse on all shifts and in some cases even a tech (“PPE Buddies”) above normal levels. The COVID patients were highly acute in isolation, required proning, and staff were constantly donning and doffing PPE, all adding extra steps to providing care. It was what was needed to survive the storm.
COVID-19 is now starting to recede into the rearview mirror, thank goodness. Society is moving toward normalcy, re-adjusting to the return of in-person learning at school, in-person work at the office, and other activities of post-pandemic living. While COVID-19 is rapidly declining in the care environments, caregiver to patient ratios are lagging in a return to normal levels. Citing Post Traumatic Stress Syndrome, Caregivers are reluctant to let their guard down. Who can blame them? Frontline staff has endured a horrifying and unrelenting experience over the past year
While the fear is easy to understand, most hospitals have lost the COVID-19 volume and the CARES ACT reimbursement that sustained them for over nearly a year and are now entering summer where volume naturally softens. Hospitals cannot afford to stay locked into the “new normal” from the past 12 months, running each unit with a higher level of staffing than is required. Nursing Staffing Matrices need to revisited, dusted off, and re-adjusted for normal caregiver to patient ratios depending on the needs of the unit. Excess personnel such as Agency and seasonal staff brought on for “leveling up” during the crisis should be eliminated immediately. This simple step is critical in the hospital industry’s own recovery from COVID-19. We can help!

Author: Betsie Sassen, R.N., M.S.N.
During COVID-19, volume in Emergency Departments across America have decreased by as much as 25-30% in some cases. The volume that has been lost is mainly lower acuity patients that found another alternative such as Urgent Care, Acute Care Clinics, or even Tele-Health. As these patients have been slowly transitioning away over the years, COVID-19 brought an abrupt halt to this type of volume coming to the Emergency Departments. These new avenues are not going away. The remaining patients are maintaining the higher acuity, and at times, even higher. In fact, our clients are reporting that while there has been a drop in volume, there has been a rise in level charges.
The challenge many are facing today is how do we look at our current standards knowing that the department “DNA” has changed. Yes, we should be adjusting our staffing down as closely as we can to the existing standard, however, do we need to re-evaluate what that standard makeup is? Is there a need for us to re-model our grids and the projected volume knowing that the average patient is carrying a higher level of care? Our advice is to reset and determine the new level of care just as if a Medical Surgical Unit switched to an Intermediate Care Unit. In that case, you would change your targets and adjust your staffing. This does not mean there are not improvements that are to be made with the volume drop, rather, the totality of the improvement might be inflated until the target has been readjusted. This is also important because many Emergency Departments have started using outside agency and higher incentive pay to compensate during the COVID-19. This needs to be cleaned up, cleaned out, and an affordable yet high quality Emergency Department must be restored.
We can help.

Author: Betsie Sassen, R.N., M.S.N.
At C2 Healthcare we’re noticing a strange phenomenon happening in hospitals across America. COVID-19 cases are dropping precipitously while other volumes are softening. Yet, hospitals are adding Travelers and Agency Nurses now at unprecedented rates. Why? Are more staff nurses leaving to join Travel Staffing Agencies? Some hospitals have decided to bring in agency to rest their staff. Again, all this happening while volume is softening, and Agency Staffing Companies have increased their hourly rates 300% and are at an all-time high…upwards of $180/hour!
Many times, departments are using agency and overtime when they are running over on the Hours Per Patient Day (WHPUOS) target. In most cases, the simple removal of agency hours would get a department to a zero variance on hours and obviously save 3 times what hours paid at straight time would be. If a department is over on its WHPUOS, agency contracts should not be renewed and in some cases cancelled with penalty. If a department is running over its target, look to see how many agency hours and overtime hours are being used, and eliminate those first to bring down the hours variance and improve cost. The cost has become so unaffordable making them “budget busters”.
Unfortunately, the pandemic has left many staff nurses feeling tired, under-appreciated, and under-valued. The lift from the “Heroes Work Here” signs and pandemic pay has worn off. Staff nurses are aware of what hospitals are currently paying agency nurses and it is creating resentment and bitterness.
If the objective of adding agency is to replace vacancies left by nurses who left to be “travelers”, what are the initiatives around trying to bring them back or stop them from leaving in the first place?
If the objective is to rest staff by adding agency, make sure the initiative is working and that your staff is indeed taking time off. Another and perhaps better question to ask yourself is if volumes are declining, is there a way to do so without adding agency?
The appeal of travel nursing will likely wear thin eventually for those who jumped ship. But, in the meantime, what is your organization doing to stop them from leaving? At C2 Healthcare we’ve seen effective “re-recruitment” campaigns of reaching out to former nurses and inviting them back. The goal is to give them an opportunity before their position is filled.

Author: Betsie Sassen, R.N., M.S.N.
As much of the country has been blanketed with snow over the last month, we are in the process of digging out using various techniques that have been used for generations. These techniques and resources have been used for many years and have worked because the challenges we have faced with weather and snow remains consistent.
However, during COVID-19 we are facing many challenges that have never been seen. Whether it is a loss of nurses to agencies, increased bonus or hazard pay, or temporary market adjustment exceeded over 30% to fight the COVID-19 battle, we now must begin the process of digging out of COVID-19 and get back to a new sense of normal.
These are all difficult challenges, like the after effect of a storm, but without a plan . . .